Meet NEFI's Lab Director
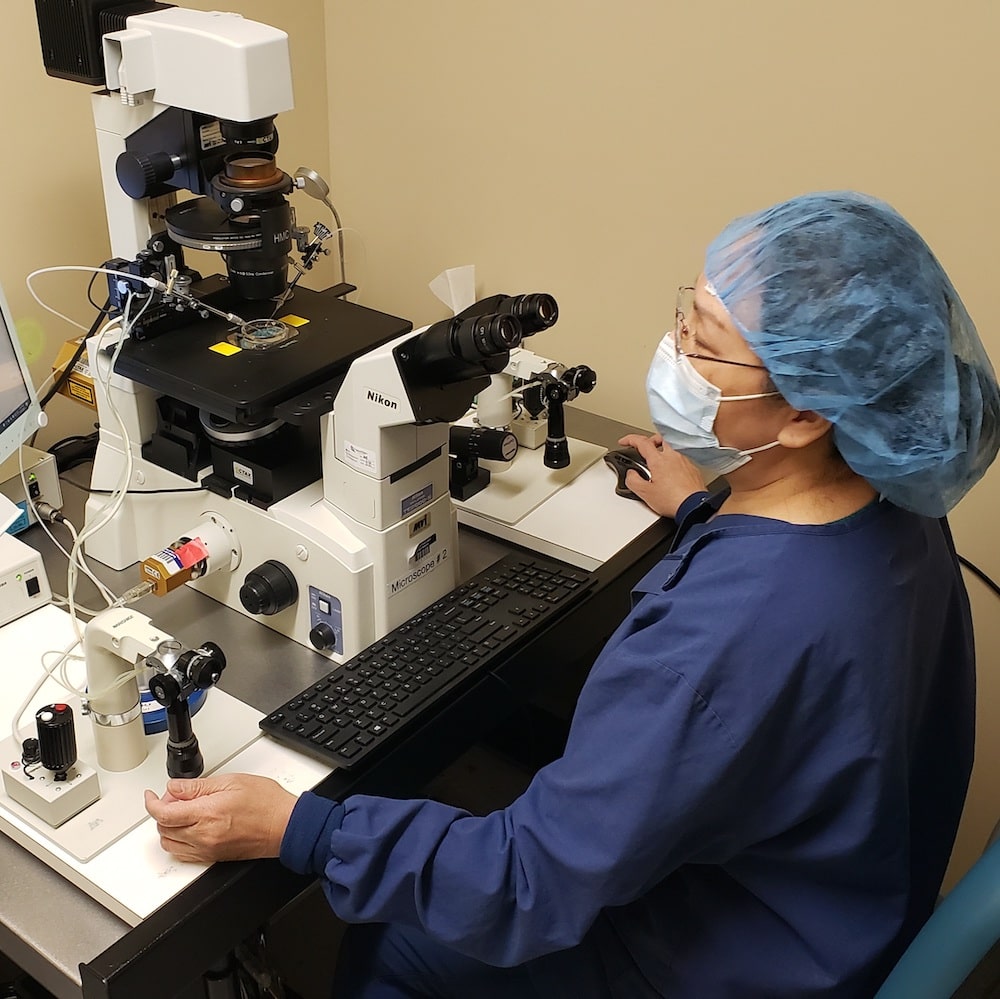
For Medical Laboratory Professionals Week, we went inside New England Fertility’s lab to get some insights from its director, Ellen She. Ellen sat down and talked to us about what happens in the lab, but also about quality control. She also shared her insights for anyone thinking about a career in embryology.
What’s your typical day at NEFI?
My schedule will vary, but various things need to be done in the lab every day, like retrievals, embryo grading, biopsies, freezing, and thawing. The very first thing we do in the morning is quality control for the entire lab and checking things like incubator temperature and gas concentration, which has a major effect on embryo development.
How and when did you get involved in embryology?
I spent 10 years as an OB-GYN and served as a medical director for four years at a fertility center in China. In 1992, I was very interested in research and went to Japan, where I got my PhD in medical physiology. After graduating, I went to Canada, where I worked with cattle embryos. Three years later, I relocated to San Diego and worked for UCSD. We studied DNA and vaccines in the cancer research field. Then I went back to embryonic research at Scripps Research institute.
If someone were just starting out in embryology, what would you tell them?
Take the time to go through all the steps and discover the purpose of what you’re doing in the lab, instead of just being taught what to do.
So, it’s like being given a recipe so you’ll know how to bake one specific cake, versus understanding the fundamentals of baking so you can bake any cake?
Exactly. That’s why a PhD is helpful. You develop analytical skills. One thing I always make sure, when training people, is to not just ask them, “Okay, what’s the next thing you need to do?” but “Why do you do it?”
That kind of approach and training sets our lab here at NEFI apart.
It does. If you know why you’re doing something, you’re less likely to make mistakes. In a lab, there’s no room for mistakes. Embryology is also such a detail-oriented field. It requires so much recording, observing, and checking — not just skill.
What are the biggest changes you’ve seen since you began working in embryology?
Mostly technical. We’re working more with male infertility, ICSI, genetic testing, and older patients, as well. We know more about genetics today, we’ve created better machines, and we have better freezing technology — today’s vitrification helps eggs recover better. Genetic sequencing also is not as difficult as it was, and, overall, protocols have improved.
There have been attempts to use artificial intelligence in embryo grading. How do you feel about it?
Technology can’t entirely replace humans. There have been attempts to make ICSI totally robotic, for example, but they haven’t been successful. Every egg and embryo is different, so even with the great technology that exists today, it requires human care to treat each egg and embryo individually.
One area where technology has made great advancements, though, is record keeping and communication with patients. The lab relies heavily on the NEFI patient portal. We also electronically keep track of everything we do, and we can collaborate with each other more easily.
What do you think will be the next frontier in reproductive science?
Breakthroughs in genetic testing and detecting mutations. I hope in the future we can create a kit that allows us to easily take culture medium and perform tests that reduce the stress on an embryo.
What is your favorite part of your job?
Seeing patients’ results. It feels great to see our hard work pay off by helping people create families.
